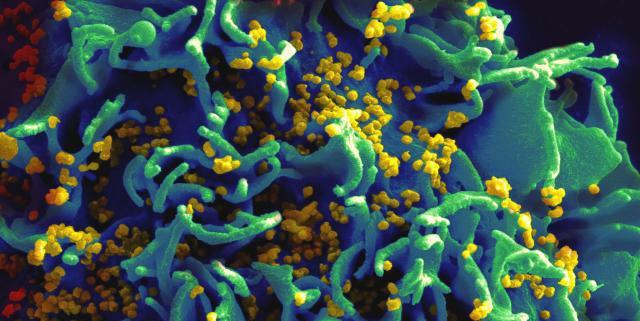
HIV and other infectious or communicable diseases
Last Updated/Reviewed: 2024
Since the California Restaurant Association (“CRA”) first published the report AIDS in the Workplace: Facts and Fears in 1985, the level of public
Please login to read the rest of this post
You must be logged in to view this resource
CRA members, please login here.
Get access to this CRA member-exclusive benefit
Thank you for your interest- This valuable resource is an exclusive benefit for California Restaurant Association Members. If you are interested in becoming a member click here to join or please contact our Member Development team at 800-765-4842 or email us at membership@calrest.org.
Need help?
Are you having trouble logging in? Please contact Jackie at helpline@calrest.org and she will be happy to assist you with your credentials.
Please note that our normal business hours are Monday through Friday 8:30am–5:00pm and we will get back to you within 1-2 business days of receiving your inquiry. Thank you for your patience and we apologize for the inconvenience.
Already have an account? Please login here.
Forgot your password? It's easy to reset it.
Request a new password